Understanding and Defining Sleep-Related Movement Disorders
Table of Contents
- Introduction: Understanding Sleep-Related Movement Disorders
- Types of Sleep-Related Movement Disorders
- Causes of Sleep-Related Movement Disorders
- Diagnosis of Sleep-Related Movement Disorders
- Treatment and Management of Sleep-Related Movement Disorders
- Conclusion: The Impact of Addressing Sleep-Related Movement Disorders
- Frequently Asked Questions
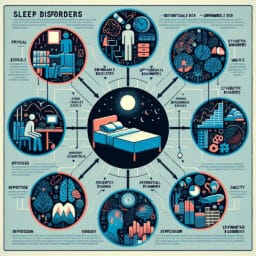
Introduction: Understanding Sleep-Related Movement Disorders
Sleep-related movement disorders are a group of neurological conditions characterized by unusual movements during sleep. These range from minor motor activity like arm twitches, to more pronounced and disruptive actions, such as rapid eye movement sleep behavior disorder. Understanding these disorders is crucial as they often lead to significant sleep disturbances and excessive daytime sleepiness, impacting one’s quality of life. Among the well-known movement disorders are Restless Legs Syndrome (RLS) and Periodic Limb Movement Disorder (PLMD). RLS triggers uncomfortable sensations usually in the legs, causing an irresistible urge to move them while trying to fall asleep. On the other hand, PLMD involves involuntary limb movements during sleep which can be simple or complex in nature — sometimes even causing periodic limb movements of the big toe. In addition to these primary types, there are also secondary variants that occur alongside other health conditions such as brain injury or stress-related issues. Remarkably, a comprehensive understanding of these abnormalities not only aids in early diagnosis through tools like sleep study but also contributes towards effective management with treatments ranging from lifestyle modifications to dopamine agonists therapy.
Types of Sleep-Related Movement Disorders
Restless Legs Syndrome (RLS), a prevalent neurological disorder, is often the culprit behind sleep disturbances. RLS is distinguished by uncomfortable sensations and an irresistible urge to move one’s legs when trying to fall asleep. These feelings may appear as a crawling or creeping sensation, typically in the lower extremities but can also affect the arm twitches. The discomfort from RLS generally worsens during periods of inactivity and at night, leading to difficulty falling asleep.
Diving deeper into another sleep-related movement disorder—Periodic Limb Movement Disorder (PLMD)—this condition involves repetitive limb movements, particularly in the lower limbs during sleep. Unlike restless legs syndrome that kicks in upon falling asleep, PLMD strikes while you’re already in slumber land with periodic limb movements such as flexing of the big toe or bending of the ankle or knee. Although these abnormal movements might not entirely wake you up from your sleep, it could lead to disturbed sleep patterns resulting in excessive daytime sleepiness.
Another common complaint among individuals suffering from movement disorders related to their sleeping pattern are leg cramps that strike them most frequently at night. These painful contractions often disrupt peaceful rest and contribute further towards restless nights.
Yet another variant of these unusual nocturnal behaviors is bruxism—the medical term for teeth grinding or clenching during sleep—which can cause not only disrupted rest but also damage to your teeth over time.
Last on our list but certainly not least—rhythmic movement disorder—is characterized by rhythmic motions including body rocking and kicking which occur right before falling asleep or even during light stages of slumber. Most common among infants and children; however, adults aren’t immune either—especially if they suffer from other neurological conditions like Parkinson’s disease or have had a brain injury.
Addressing these myriad forms of Sleep-Related Movement Disorders effectively requires comprehensive knowledge about each type along with their risk factors—which range from genetic predispositions through health conditions such as iron deficiency or neuropathy, to lifestyle factors like diet, caffeine, alcohol consumption, and the use of illegal drugs. By understanding these disorders better and seeking appropriate sleep medicine intervention from a specialist in this field, not only can sleep be improved but so can overall quality of life.
| Sleep-Related Movement Disorders | Description | Common Symptoms | Common Risk Factors |
|---|---|---|---|
| Restless Legs Syndrome (RLS) | A prevalent neurological disorder characterized by uncomfortable sensations and an irresistible urge to move one’s legs when trying to fall asleep. | Crawling or creeping sensation in the lower extremities, difficulty falling asleep. | Genetic predispositions, iron deficiency, lifestyle factors such as caffeine and alcohol consumption. |
| Periodic Limb Movement Disorder (PLMD) | Condition involves repetitive limb movements, particularly in the lower limbs during sleep. | Periodic limb movements such as flexing of the big toe or bending of the ankle or knee, disturbed sleep patterns, excessive daytime sleepiness. | Genetic predispositions, health conditions such as neuropathy, lifestyle factors like diet, alcohol consumption and use of illegal drugs. |
| Leg Cramps | Painful contractions often disrupt peaceful rest and contribute further towards restless nights. | Nighttime leg cramps, disrupted sleep. | Health conditions such as iron deficiency, lifestyle factors like diet and alcohol consumption. |
| Bruxism | Teeth grinding or clenching during sleep. | Disrupted sleep, damage to teeth over time. | Health conditions such as stress, lifestyle factors like alcohol consumption and use of illegal drugs. |
| Rhythmic Movement Disorder | Characterized by rhythmic motions including body rocking and kicking which occur right before falling asleep or during light stages of slumber. | Body rocking, kicking, disrupted sleep. | Other neurological conditions like Parkinson’s disease or brain injury, genetic predispositions. |
Causes of Sleep-Related Movement Disorders
Surprisingly, genetics play a significant role in the occurrence of sleep-related movement disorders, such as restless legs syndrome and periodic limb movement disorder. Various studies in sleep medicine have revealed that these neurological disorders often run in families, hinting at a strong genetic link. The complex interplay of multiple genes likely contributes to the manifestation of such conditions.
Lifestyle factors also have a substantial impact on triggering symptoms or making them worse. For instance, excessive intake of caffeine or alcohol, poor diet, and use of illegal drugs can exacerbate the uncomfortable sensations associated with arm twitches or periodic limb movements experienced during sleep. The resulting sleep disturbances may then lead to excessive daytime sleepiness and further health complications if left unaddressed.
Medical conditions constitute another critical component contributing to these disorders. Certain health conditions like iron deficiency, neuropathy, Parkinson’s disease or brain injury stress can instigate abnormal movements during slumber or complicate existing issues like restless legs syndrome or rapid eye movement sleep behavior disorder. It’s important for individuals experiencing consistent disruptions in their sleeping patterns due to minor motor activity or more pronounced actions to undertake a comprehensive sleep study for an accurate diagnosis.
In essence, comprehending the full scope of risk factors involved—ranging from genetic predispositions through lifestyle influences to health issues—is pivotal for effective management and treatment using approaches such as dopamine agonists therapy or lifestyle modifications as necessary.
Diagnosis of Sleep-Related Movement Disorders
A sleep study, also known as polysomnography, is a critical tool in diagnosing sleep-related movement disorders. It monitors brain waves, oxygen levels in the blood, heart rate and breathing rate during sleep cycles to capture any abnormal movements or patterns that may be disrupting restful slumber. This includes periodic limb movements such as arm twitches or flexing of the big toe and rapid eye movement sleep behavior disorder—conditions that often cause significant sleep disturbances which lead to excessive daytime sleepiness. Interestingly, these neurological disturbances are not isolated events but commonly occur alongside restless legs syndrome (RLS), illustrating the interconnected nature of these disorders.
The importance of medical history in detecting these conditions cannot be overstated. Certain risk factors like genetic predispositions could provide vital clues towards an accurate diagnosis since many well-known movement disorders run in families. Additionally, lifestyle factors such as diet, caffeine or alcohol consumption and use of illegal drugs can trigger symptoms and make them worse.
Similarly essential is a thorough physical examination. Specific health conditions like iron deficiency or neuropathy can instigate abnormal movements during slumber, making it imperative for physicians to evaluate patients for related signs meticulously. In essence, comprehensive analysis through tools like a sleep study along with careful evaluation of one’s medical history and physical health status form the bedrock for effective diagnosis and management of these complex types of neurological disorders.
Treatment and Management of Sleep-Related Movement Disorders
A remarkable aspect of tackling sleep-related movement disorders is that while medication plays a pivotal role, simple lifestyle changes can also significantly alleviate symptoms. For instance, curbing excessive caffeine or alcohol intake and eliminating the use of illegal drugs can remarkably mitigate uncomfortable sensations tied to restless legs syndrome or periodic limb movements during sleep. Further, dietary improvements could potentially counteract health conditions like iron deficiency that trigger abnormal movements in slumber.
Intriguingly, incorporating specific therapies into one’s routine has shown promise in managing these neurological disorders. Techniques such as cognitive-behavioral therapy focus on altering thought patterns to mitigate disturbances linked with falling asleep. Additionally, physical exercises might help subside the minor motor activity seen in these disorders and improve overall sleep quality.
On the pharmaceutical front, dopamine agonists emerge as an effective treatment for mitigating symptoms associated with well-known movement disorders like primary PLMD and RLS. These medications work by regulating dopamine—a neurotransmitter responsible for controlling bodily movements—that often run awry in these conditions.
While understanding sleep-related movement disorders appears daunting due to their complex nature and wide array of risk factors involved; remember—an informed approach encompassing appropriate therapies combined with lifestyle modifications can pave the way towards successful management—and more restful nights ahead.
Conclusion: The Impact of Addressing Sleep-Related Movement Disorders
Despite their complexity and daunting array of risk factors, understanding sleep-related movement disorders like Restless Legs Syndrome (RLS) and Periodic Limb Movement Disorder (PLMD) holds the key to unlocking restful nights for countless individuals. The gnawing discomfort that accompanies these disorders—whether through periodic limb movements or minor motor activity—isn’t just a mere nuisance; it can lead to significant sleep disturbances wreaking havoc on an individual’s quality of life. It’s crucial not to underestimate the power of early diagnosis using tools such as sleep study in capturing abnormal movements during slumber. Interestingly, treatment isn’t always reliant on strong pharmaceuticals like dopamine agonists. Simple lifestyle changes—like reducing caffeine intake or incorporating physical exercises—can also dramatically alleviate symptoms and improve overall sleep quality. By empowering patients with knowledge about their condition and providing them with practical strategies for its management, we open doors to more peaceful nights and, consequently, healthier days—a testament to the transformative potential of effective sleep medicine.